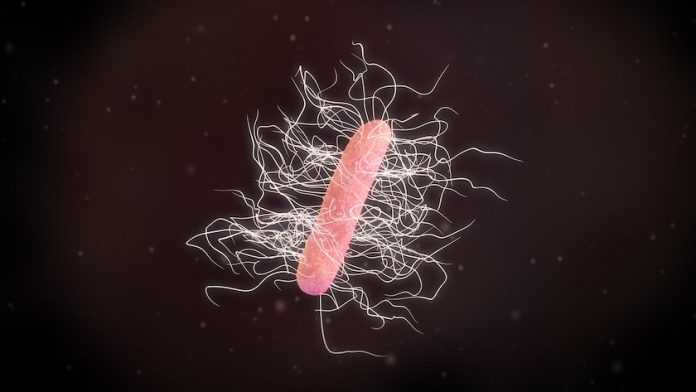
One of the most notorious bacterium you may be familiar with is Clostridium difficile, also known as C. diff. The presence of Clostridium difficile has become nearly synonymous with antibiotic resistance, since it is one of the bacterium that is resistant to this class of drugs. This drug resistance is associated with the deaths of approximately 23,000 people in the United States who contract a C. diff infection every year, some of which are acquired during hospitalization. C. diff is normally spread through fecal-oral contact, meaning oral contamination by bacteria from fecal matter, either directly by hand contact, or indirectly through various food or water sources. Hospitals are one of the most common sites for C. diff contamination.
Also read about reducing hospital acquired infections
C. difficile are incredibly resilient. When the good bacteria in your intestinal tract keep these bad boys under control and in low numbers, all is well. However, if you take an antibiotic, the good bacteria are attacked and may no longer be able to protect against C. diff infection. In fact, C. diff produce spores when they encounter antibiotics, and these spores can live for as long as two years, long after the bacteria have been eliminated. That’s why if you wipe out a C. diff infection with medication, the condition may return.
How C. diff affects digestion
If you contract a C. diff infection, you may experience symptoms that range from mild to severe. Initial symptoms usually include stomach pain and watery diarrhea, after which you can advance to more severe symptoms including fever, nausea, vomiting, weakness, swollen abdomen, watery diarrhea 10 or more times daily, rapid heart rate, elevated white blood cell count, and dehydration. As the condition grows worse, your intestinal tract will become inflamed to the point that you may be unable to expel gas and stool, which is life-threatening.
In a mouse study published in Infection and Immunity, researchers made a significant discovery about how C. diff works in the body. When the scientists introduced the bacteria into the mouths of mice, they found that it took only 24 hours for the spores to turn into diarrhea-inducing cells. They also found that the bile acids present in the gut of the mice triggered the C. diff spores, which caused them to grow into cells that populate the small intestine within 24 hours. All of this information may prove helpful in deciding how to successfully treat C. diff infections in the future.
For now, however, our knowledge of C. diff has not advanced as far as many had hoped. Therefore, we continue to look for effective, safe way to prevent and treat this serious condition.
How is C. diff diagnosed and treated?
If you experience some of the symptoms of C. diff infection, you need to consult your doctor and get a lab test, which involves an evaluation of your stool. A gastroenterologist can determine if you have a C. diff illness. If the answer is yes, the doctor may perform an inspection of your intestinal tract using a colonoscope to look for any damage and the presence of fleshy growths on the wall of the colon (polyps).
For anyone who has a challenging case of C. diff, it is best to seek the advice of a gastroenterologist who is familiar with the disease. Some of the most recommended natural remedies for C. diff infections are the following:
Stop taking antibiotics. The Food and Drug Administration recommend that you stop all antibiotic treatment if you have C. diff. You may notice a significant improvement fairly quickly.
Consume probiotics. Whether you eat foods that are rich in beneficial bacteria (such as sauerkraut, kimchee, kefir, tempeh, kombucha, raw apple cider vinegar, yogurt), take probiotic supplements, or both, providing your intestinal tract with good bacteria is the goal so you can best combat these nasty bacteria.
Avoid or limit certain foods. Some foods are best avoided if you have or suspect you have a C. diff infection. They include fatty/greasy foods, dairy products, raw fruits and vegetables (cook them first), processed fat-free foods (they can cause bloating), spicy foods, lots of caffeine, and certain gas-producing foods such as cruciferous vegetables, nuts, seeds, beans, and whole grains.
Wash your hands. If you already have a C. diff infection, it is highly recommended you wash your hands thoroughly to help prevent spread of the infection. Plain soap and water is sufficient; antibacterial soaps are not recommended, even by the FDA.
Read about how to reduce the spread of germs
Enjoy natural antibiotics. Prescribed antibiotics are the typical way doctors try to manage C. diff, but natural antibiotics are a possible alternative way to go. Talk to a knowledgeable healthcare provider about the value of using raw garlic, Manuka honey, and oil of oregano to help support the immune system against C. diff infection.
Keep it shut. One simple yet effective way to help prevent reinfection or the spread of C. diff is to always shut the lid of the toilet before you flush. This is a habit that should be impressed upon all members of your family. Naturally, you likely won’t be able to do this in public restrooms, but always strive to do it at home.
Eat poop. Research into the value of fecal transplants has shown that taking a supplement of freeze-dried fecal matter in capsules can prevent recurrence of C. diff infection for two months. Further research is necessary to determine whether this approach has staying power. There is a surgical approach to fecal transplant as well.
[Editor's Note: Our partner Bio-K+ offers a 100% probiotic product with proven benefits and effectiveness on human health. Bio-K’s probiotic helps to maintain a healthy intestinal flora, support intestinal functions and activate your immune system. They have a wide range of products for your needs including fermented drinkable products for adults and children as well as capsules. For more healthy inspirations, visit Bio-K+ blog.]
Sources
Food and Drug Administration. Antibacterial soap? You can skip it, use plain soap and water.
Healthline.com. What are the most effective natural antibiotics?
Koenigsknecht MI et al. Dynamics and establishment of Clostridium difficile infection in the murine gastrointestinal tract. Infection and Immunity 2015 Mar; 83(3): 934-41
Staley C et al. Successful resolution of recurrent Clostridium difficile infection using freeze-dried, encapsulated fecal microbiota; pragmatic cohort study. American Journal of Gastroenterology 2017 Jun; 1126): 940-47










